
Yeast Antibodies Predict More Severe AS
March 25, 2008ISTANBUL, Turkey—Saccharomyces cerevisiae, the yeast used in bread and beer, may also provide a handy immunologic marker that predicts more severe disease in patients with seronegative spondyloarthropathies.
Sibel Zehra Aydin, MD, and colleagues at Marmara University in Istanbul, Turkey, reported in Rheumatology that anti-Saccharomyces cerevisiae antibodies (ASCA) are significantly more prevalent in patients with ankylosing spondylitis (AS) or undifferentiated spondyloarthropathies (uSpA) that in healthy controls.1
{}“ASCA can also be a marker of radiological damage and a more severe course in AS,” Dr. Aydin said.
The researchers suggest that AS patients with more advanced disease may have increased intestinal involvement, and that ASCA positivity reflects higher disease activity as a marker of ongoing antigenic stimulus. A second possibility is that high ASCA levels are a sign of increased intestinal permeability, which could cause more radiological damage as a result of ongoing antigenic stimulation.
“In our study, we have shown that ASCA-positive patients had radiologically more severe disease and required anti-TNF therapy more frequently, and although statistically not significant, [they] had reduced chest expansion and higher BASFI (Bath Ankylosing Spondylitis Functional Index) scores,” Dr. Aydin said.
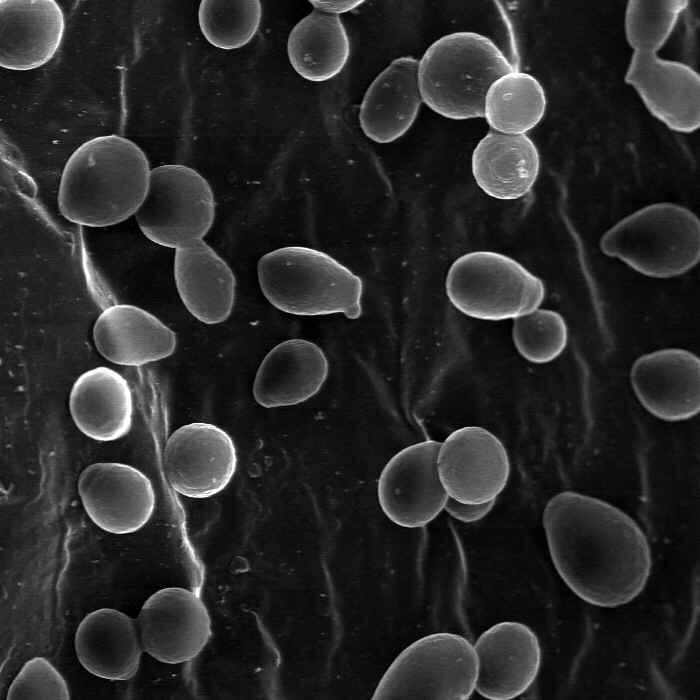
Antibodies against the yeast Saccharomyces cerevisiae
are more prevalent in AS and undifferentiated SpA,
and are associated with worse radiological damage
and a more severe disease course.
The researchers measured ASCA immunoglobulin A (IgA) and immunoglobulin G (IgG) levels in 175 AS patients, 47 uSpA patients, and 103 healthy control subjects. They found that
- ASCA IgA was positive in 20.6% of AS patients vs 5.8% of controls (P = .0008)
- ASCA IgG was positive in 10.9% of AS patients vs 5.8% of controls (P = .2)
- Either ASCA IgA or IgG was positive in 26.9% of AS patients vs 10.7% of controls (P = .001)
- Median chest expansion was 2.5 cm in AS patients vs 3 cm in controls (P = .076)
- Median BASFI score in AS patients who were positive for either ASCA IgA or IgG was 7 vs 5.5 in controls (P = .037)
- ASCA-positive patients were significantly more likely to need anti-TNF therapy compared with ASCA-negative patients (P = .0006)
ASCA positivity was not influenced by HLA-B27 positivity, age, or disease duration. “As our study is cross-sectional, whether ASCA presence is the result of or a pathogenic factor for disease severity and radiological damage is unclear,” Dr. Aydin said.
Reference
1. Aydin SZ, Atagunduz P, Temel M, et al. Anti-Saccharomyces cerevisiae antibodies (ASCA) in spondyloarthropathies: a reassessment. Rheumatology. 2008;47:142-144.