“The material that we put in there comes to life and biointegrates with the bleeding bone.”—Scott Steinman, MD
Dr. Steinman described the new treatment in a press briefing at the American Academy of Orthopaedic Surgeons 2009 meeting.1“The most common area in the hand for arthritis is the joint at the base of your thumb, and it can produce quite debilitating pain,” Dr. Steinman said. He noted that any procedure that would be proposed as an alternative to the traditional open-incision approach to treating thumb OA should be minimally invasive, should not alter the native anatomy much, and should address the central problem (in this case the arthritis).
Bleeding bone brings healing elements into thumb joint
Previous non-arthroscopic procedures have typically changed the basic anatomy of the wrist by totally or partially removing parts of the bone. Dr. Steinmen and colleagues have replaced that approach with arthroscopic carpo-metacarpal (CMC) interposition arthroplasty in many cases.
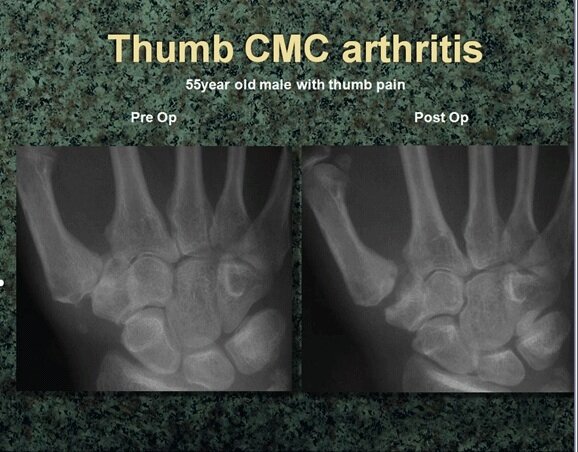
Pre-operative (L) and post-operative (R) views of arthroscopic carpo-metacarpal (CMC) interposition arthroplasty used to treat OA in a 55-year old male.
“When you look at the radiography of these patients, you see that the joint cartilage is gone. It is normal to have spaces in the joint, which are actually cartilage. When you see bone-on-bone, you know the cartilage is gone. Our approach is to resurface it. There are several materials on the market that can be used for this purpose,” Dr. Steinman said.
After entering the wrist from two angles, Dr. Steinman uses a burr to debride 2-3 mm of arthritic bone from the damaged surface on one side of the arthritic joint. “The bone underneath is cancellous bone, which bleeds and can bring healing elements into the joint itself,” he said.
Next, Dr. Steinman interposes a small cushion of collagen, which he calls “poor man’s cartilage,” in between the two bones to prevent bone-on-bone contact. “The material that we put in there comes to life and biointegrates with the bleeding bone. It then becomes the native interposition in that patient,” he said. This restores the protective cushion between the joint surfaces, reduces pain, and restores function, he said.
“Thumb carpo-metacarpal arthroscopic debridement and interposition are helpful for OA. There are not prospective studies to date compared to open procedures. But patients sure like the two small little holes!” Dr. Steinman concluded.
Reference
1. Steinman, S. A new treatment for thumb arthritis. Press briefing presented at the AAOS 2009 meeting, Las Vegas, February 26, 2009.






