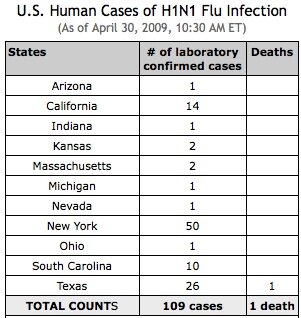
 The swine flu is a respiratory infection caused by influenza type A viruses (swH1N1) that typically cause outbreaks of influenza in pigs. Person-to-person transmission has now been reported in California, Texas, Kansas, Ohio, Mexico and New York City. The cases in Mexico have had a high mortality rate even among the young, but the confirmed cases in the US have been mostly mild.
The swine flu is a respiratory infection caused by influenza type A viruses (swH1N1) that typically cause outbreaks of influenza in pigs. Person-to-person transmission has now been reported in California, Texas, Kansas, Ohio, Mexico and New York City. The cases in Mexico have had a high mortality rate even among the young, but the confirmed cases in the US have been mostly mild.The Department of Health and Human Services has declared the swine flu outbreak a public health emergency, and the World Health Organization (WHO) has raised its pandemic alert level from level three to level four on the WHO's six-level threat scale.
“This is a serious infection and people with rheumatic and autoimmune diseases taking immunosuppressant agents are at high risk for infections and for the infections to be severe, so they are definitely at higher risk for swine flu [and swine flu-related mortality],” warned Eric Matteson, MD, professor of medicine at the Mayo Clinic in Rochester, Minnesota. “Patients with these diseases should be concerned if they have come into contact with identified cases, and it is prudent to contact your provider if you have been in contact with an identified case,” Dr. Matteson said.
Swine flu risk in rheumatology patients: be prudent, not paranoid
“This is a serious infection and people with rheumatic and autoimmune diseases taking immunosuppressant agents are at high risk for infections and for the infections to be severe, so they are definitely at higher risk for swine flu [and swine flu-related mortality].”—Eric Matteson, MD
Anti-viral drugs such as Tamiflu (oseltamivir) can treat the swine flu, but “don’t stockpile Tamiflu because this can cause a ‘panic and run’ in available supplies and then the people who have had exposure may not get the drug,” Dr. Matteson cautioned. “The antivirals should be provided to people who have had exposure and to identified cases only.”Rheumatologists, like all doctors, need to be virus-trackers.
“Providers should be aware whether the swine flu is spreading in their area. If it is, inquire if your patients have been in contact with any cases or if they are having symptoms and signs,” Dr. Matteson said.
The symptoms of swine flu include fever, cough, sore throat, body aches, headache, chills, fatigue, diarrhea and vomiting.
If swine flu is suspected, the federal Centers for Disease Control and Prevention (CDC) in Atlanta states that physicians should obtain a respiratory swab for swine influenza testing and place it in a refrigerator. Once collected, contact the state or local health department to facilitate transport and timely diagnosis at a state public health laboratory.
“Essentially, we don’t know whether we have an epidemic, pandemic or nothing at this point, but everybody should be screened for this flu if they have signs, symptoms and some connection to places where there are outbreaks, especially those who are immunocompromised such as patients taking steroids to treat rheumatic or autoimmune diseases,” said E. Neil Schachter, MD, professor of medicine and community medicine and the medical director of the respiratory care department at the Mount Sinai Medical Center, in New York City.
Prevention is essential in the face of a potential swine flu pandemic. The CDC states that the best way to stave off swine flu is with frequent hand washing using soap and water, especially after coughing or sneezing and/or usage of alcohol-based hand cleaners, avoiding close contact with sick people and staying home if you are sick.






